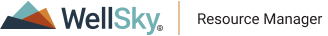
Reimbursed Column
The Reimbursed column is one of two locations where users can enter the expected reimbursement amount for an appointment when the appointment has an associated authorization that has been defined to manually calculate reimbursements amounts. Only appointments with such an authorization can use the "reimbursement" feature. Physical or Speech Therapy clinics offer a typical example for how this feature can be used in regard to managing Medicare benefits. For example, the clinic can
- Create a money authorization based on the benefit cap (e.g., $1880.00), which includes the option to
- Enter any previous benefit provided at another clinic as "Initial Money," and which is in turn used to calculate the remaining benefit balance.
- Set a threshold at which to warn users that the patient is approaching the cap on their benefit.
- Then, as a patient receives treatment, whoever is responsible in the care workflow can enter expected reimbursement amounts against a patient's completed appointments, which will in turn decrement money from the total remaining benefit on the authorization.
To use the feature:
- Navigate to the Check-in screen.
- Click the Reimbursed field in the appropriate appointment line item.
- Enter the expected reimbursement for the specific appointment and then press the Tab or Enter key on the keyboard to commit your change. (If you click away, your change will not be saved.)
- Continue with additional check-in tasks as necessary.
If the appointment has not been marked Arrived or Seen, you must check it in before applying a reimbursement amount.
Keep in mind that if the appointment does not have an authorization or an authorization of the appropriate type, then this field will not be exposed and users won't be able to enter an amount. Consider the appointment for Ashley Elmwood in the previous illustration.
An alternative workflow for entering expected reimbursements is provided on the grid in the scheduling palette. See the Expected Reimbursement Amount topic for the steps.
Key Considerations about Entering Reimbursement Amounts
- In order to apply reimbursement amounts to an appointment, users must first have "Edit Appointment" rights and "Change Appointment Status" set to Full in their security profile.
- The patient (a) must have a money authorization and (b) the "calculate reimbursement" option must be enabled on that authorization, and (c) the authorization must be associated with the appropriate appointments. Otherwise, the reimbursement field will not even appear on the palette or in the Check-in screen.
- Money is decremented from the authorization when a reimbursement amount is entered for an appointment. Remember that money authorizations that do not have the option enabled are decremented by the dollar amount assigned to any associated procedures on the appointment when that appointment is checked in (marked Arrived or Seen).
- Reimbursement amounts can be applied to appointments for Today's date or earlier. You cannot apply them to appointments in the future.
- Users can track expected reimbursement amounts by appointment by generating the Estimated Reimbursement Tracking report.
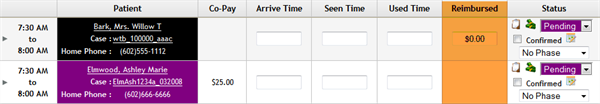
- If the status of the appointment is Pending, a pop-up dialog similar to the following will appear when the reimbursement is entered:
- If the expected reimbursement exceeds the authorized amount, a warning similar to the following will appear:
If you click OK, the appointment status will be changed to Seen for the current time. If (a) the reimbursement amount is entered at a time other than when the patient was actually seen and (b) the exact time at which the patient was seen is required, then change the time on the Check-in screen.
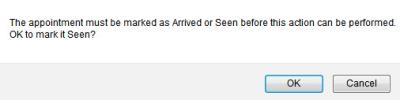
If you change the status of an appointment with a reimbursement from Arrived or Seen back to Pending, the reimbursement will be erased:

Click OK to continue, Cancel to abort the reimbursement application. Keep in mind that the security profile assigned to the user must have "Book Beyond Max Visit Count of Auth" set to Full in order to enter an amount that exceeds the authorization.
- Although money authorizations that have the "Manually calculate reimbursement amount" option enabled only decrement from the authorization according to what users enter against appointments with which the authorization is associated, procedures that have an associated cost in their definition are also used to provide an estimate of the potential reimbursement amount by which to decrement the authorization. Consider the following example:
- Patient A has an authorization for $1000.00 and the manual calculation option is enabled.
- The patient has two previous appointments in which (a) one is marked Seen and has an expected reimbursement of $500.00 and (b) one is still Pending but has an assigned procedure (say 99010) with an associated cost of $100.00.
- If a third appointment is scheduled for the patient and a procedure with an associated cost of $300.00 is assigned to the appointment, a message similar to the following will appear:
$500/$1000 used and $100 estimated pending, this will result in $300 estimated usage.
Where (a) $500 is the expected reimbursement entered for the first appointment, (b) $100 is the estimated reimbursement based on the potential charge for the procedure on the existing pending appointment, and (c) $300 is the estimated reimbursement based on the potential charge amount for the procedure on the appointment currently being scheduled.
An estimated reimbursement is logged against a money authorization only when procedures that have an associated cost are assigned to the appointment. Otherwise, there is nothing on which to base the estimate.