Authorization Types
Authorizations Based on Visits
Initial Visits: If the patient is new to the scheduler, but is in the middle of a series of authorized treatment, simply enter the number of visits he or she has used prior to being scheduled in the program in the Initial Visits field. The program will use this number as part of the calculation for Used Visits.
Used Visits: This field is calculated automatically using the following formula:
Used Visits = Initial Visit + CompletedAppointments
(where completed appointments are those that have been marked Arrived or Seen)
Reference the statistic to prevent unbillable/unauthorized treatment and to alert the appropriate resources that a patient's treatment plan requires attention.
Authorized Visits: Enter the approved number of visits in the Authorized Visits field.
Consider, for example, a patient who has 15 authorized visits and is entered into the program after he or she has completed 5 of those visits. When creating the authorization you would not enter 5 in the Initial Visits field and 10 in the Authorized Visits field; rather, you would enter 5 in the Initial Visits and 15 in the Authorized Visits field.
Number of Visits to warn before: This field represents the threshold at which you want a conflict alert to pop up to warn whoever may by scheduling the patient that their authorization is nearing its treatment limit. This is different than the warning that will occur if the authorization has expired. Simply enter the value that fits within your business workflow for contacting patients, providers, and insurance companies.
Key Considerations
- Important! A patient’s appointments must be marked Arrived or Seen to be included in the authorization calculation. Otherwise the authorization is not decremented.
Authorizations Based on Days/Weeks
Authorizations based on Days and Weeks are basically the same, with the only difference being the length of the time metric (i.e., a day versus a week).
Initial Days/Weeks: As with Visits, the "Initial" field represents treatment that the patient may have received prior to being scheduled in the program. If this situation occurs, enter the number of days/weeks of treatment the patient has received here.
Days/Weeks Used: A day or week has been used if the patient has completed an appointment within that day or week. A week is defined by the normal workdays for the organization or domain.
Consider a patient that has been authorized for four weeks of treatment. He or she can be treated once or 500 times during a given week. Either way the week will be counted as used. If the patient skips a week, that week is not counted. This is not the same as when the authorization expires.
Authorized Days/Weeks: Enter the number of days or weeks of treatment for which a patient has been authorized.
Number of Days/Weeks to warn before: Enter the appropriate threshold that will trigger a conflict warning that the patient is nearing the end of his or her authorized treatment.
Key Considerations
- A patient’s appointments must be marked Arrived or Seen to be included in the authorization calculation. Otherwise, the authorization is not decremented.
Money ($) Authorizations
Initial Money: Enter the dollar amount for the treatment that the patient has received prior to being scheduled in your organization, or before the authorization was input into your system. For example, the patient or insurance company (or whoever is responsible for paying) may have authorized $2500.00 of treatment for a given case. The patient may have already used $500.00.
Money Used: The money used calculation is based on either:
- Simple money authorizations are decremented when procedures that have an associated cost/charge are assigned to the appointments that are associated with the authorization. An authorization could be associated with 10 appointments, for example, but if none of those appointments has an associated procedure that is defined with a dollar cost, nothing will be decremented from the authorization.
- Money authorizations that have the “manually calculate reimbursement amount” enabled are decremented by the expected reimbursements that are entered against each appointment—see the following option.
Manually Calculate Reimbursement Amount: Enable this option if you have a situation in which you need to track the expected reimbursement for each appointment against a money authorization.
For example, an outpatient PT office could create a therapy cap authorization ($1880.00) to monitor the expected reimbursement against the therapy cap imposed by Medicare. For example,
- Assign the authorization to the appropriate appointments.
- Then enter the expected reimbursement against each visit, which will (i) decrement the authorization and then (ii) warn users at a predetermined threshold when the patient’s Medicare benefit is nearly exhausted.
Authorized Money: Enter the authorized dollar amount for the treatment.
Amount to warn before: Enter the threshold (in dollars) that will trigger a conflict warning that the patient is nearing the end of his or her authorized treatment.
Key Considerations
- In general, money is decremented from the authorized amount based on the procedures that are scheduled for the patient. Only procedures that are associated with a dollar amount will decrement the authorization, and then only when the associated appointments have been checked in. The key exception is if the "manually calculate” option is enabled. In such instances, money will decrement only when the expected reimbursement is entered against each appointment manually.
- Although money authorizations that have the "manually calculate" option enabled only decrement from the authorization according to expected reimbursement entered against appointments that use the authorization, procedures that have an associated cost in their definition are used to provide an estimate of what potentially may be charged against the authorization. Consider the following example:
- Patient A has an authorization for $1000.00 and the manual calculation option is enabled.
- She has two previous appointments where the first is marked Seen and has an associated charge of $500.00 and the second is still Pending but has an assigned procedure (say 99010) with an associated cost of $1.00.
- If a third appointment is scheduled for the patient and a procedure with an associated cost of $300.00 is assigned to the appointment, a message similar to the following will appear:
$500/$1000 used and $100 estimated pending, this will result in $300 estimated usage.
Where (a) $500 is the charge entered for the first appointment, (b) $100 is the estimated charge for the existing pending appointment, and (c) $300 is the estimated charge for the appointment currently being scheduled.
An estimated reimbursement is logged against a money authorization only when procedures that have an associated cost are assigned to the appointment. Otherwise, there is nothing on which to base the estimate.
- Expected reimbursements can be entered against authorizations that have the "manually calculate" option enabled (a) only for appointments that occur on or before Today and (b) only once they have been checked in.
Procedure Authorizations
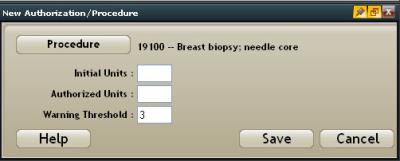
Authorizations may be issued for a specific procedure or set of procedures. When a procedure authorization is created, at least one procedure is required to save it. A procedure authorization cannot exist without an assigned procedure.
- Click the Add button once the Procedure option has been selected. A Procedure Search screen will appear:
- Navigate to and select the appropriate procedure. The New Authorization/Procedure screen will appear. Verify the correct procedure was selected. Alternatively, click the Procedure button to select the correct item.
- Enter the following information:
- Number of times the procedure was completed for the patient prior to being scheduled in the program in the Initial Units field.
- Number of times the patient has been authorized to receive the procedure in the Authorized Units field.
- Threshold at which users should be warned that the patient's authorization is nearing completion in the Warning Threshold field.
- Click Save to commit the record. Click Cancel to abort it.
- Repeat steps 1–3 as necessary.
As appointments are scheduled for this patient case, then, the “procedure” authorization will be made available in the Edit Appointment screen.
If, however, you attempt to use the authorization without selecting the appropriate procedure, a conflict will appear and you will not be able to schedule the appointment until you either remove the authorization or select at least one procedure that meets the parameters of the authorization.
Key Considerations
- Unless the procedure for which a procedure authorization is created is actually scheduled for a patient, the authorization will not apply, and the units will not be decremented.
- The appointment for which a procedure authorization is scheduled must be marked Arrived or Seen for the authorization to decrement appropriately.